Engagement
Create solutions to reach and interact with members effectively to increase loyalty, retention, and branding.

.png)

Create solutions to reach and interact with members effectively to increase loyalty, retention, and branding.

Enable team collaboration and productivity by providing solutions that streamline communication, automate workflows, and improve access to information.

Unite data silos and apply advanced analytics and AI to reveal actionable insights to help make better, faster decisions on claims and operations.
Automate claims processing to reduce claim service inventories, process appeals/denials/grievances, and automate pre-authorizations.
Create a world class contact center, self-service channels, and support services for member enrollment, on-boarding, member inquiries, and proactive communication.
Automate audits for enrollment, claims, self-service, manual inquiries and first call resolution.
Automate provider data management, provider onboarding, and provider data confirmation.
Streamline and automate shared support services that include IT, finance, HR, and legal.
According to a leading industry report, $7 billion in operating income can be unlocked by healthcare payors in areas like Claims, Membership Management, Customer Interactions, and Provider Data Management. Lateetud discusses the challenges and opportunities faced by healthcare payors.
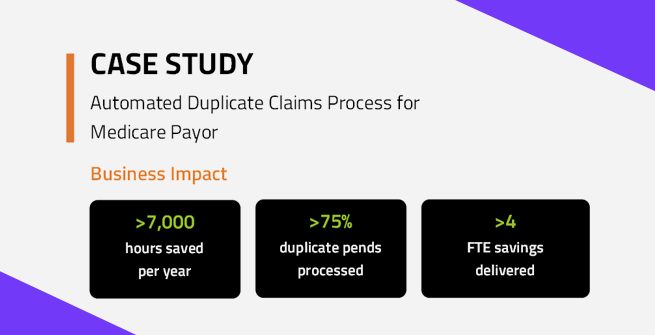
Nation's leading healthcare payor processes over 51K duplicate claims per month, saving over 7,000 man hours through automation.