
Role of RPA in Revolutionizing Revenue Cycle Management of Healthcare
- Pawan Jadhav
- January 8, 2021
The healthcare around the world is battling two different crises at present - one the deadly COVID-19 pandemic and the other; the financial turbulence. Although the end for the pandemic is at the hands of the healthcare itself, for the later; automating its Revenue Cycle Management via Robotic Process Automation is the most needed cure.
None of us imagined that the zest with which we welcomed the year 2020 would turn out to be so traumatic with the invasion of the deadly virus COVID-19. Although we are about to bid farewell to this unfortunate year; we are still clueless about getting freedom from the pandemic.
COVID-19 has undoubtedly tossed everything upside down. It has affected us all physically, mentally, socially, and the worst - economically, but it is the businesses that are experiencing the adverse effects of it. Social distancing, lockdowns, restrictions, curfew, every industry sector is the victim of the pandemic, but it is the healthcare that is the worst-hit of all. Hence, it is time to bring the most-needed change in healthcare to lessen the load on it to some extent.
The Need for Automating Healthcare Process

The COVID-19 outbreak is a wakeup call for us, humans, to realize how much more important health is than all the luxuries in the world and hence; our healthcare system needs to be updated with the latest technologies to be able to stand against any such adverse event. So, what can be done you may think?
Well, we all know how much paperwork it takes behind a doctor visit. From taking an appointment, consulting an expert, filing records, conducting tests, admitting, discharging, to billing, there are a lot of procedures to be followed which is done manually till today and which is putting a colossal strain on our healthcare system as the many valuable hours and manual labour are getting wasted in carrying out such repeated and menial tasks.
According to McKinsey Quarterly statistics, 36% of the healthcare tasks — mostly, managerial and back-office can be automated. There, RPA (Robotic Process Automation) is just what we need which is a form of business process automation that performs error-free repetitive tasks with the help of software bots, round-the-clock, thereby reducing human intervention in routine tasks.
What is RCM?
Hospitals and health systems are not just about treating patients, in fact, behind the scenes of a patient coming to the hospital till leaving it is the real deal. There are a lot of non-medical works which include taking care of all the documentation, eligibility verification, demographic entry, billing & coding and filing of the medical claims that take place in large numbers daily, is nothing but RCM.
Revenue Cycle Management is the administration of the essential financial processes in healthcare like identifying patient’s personal information, collecting payments, insurer name and treatment codes along with financial billing information, and managing the revenue generated from payers based on the services provided. Since medical claims are significant for both the patients and healthcare; an accurate and efficient RCM is required which can be achieved and made easy with RPA but before that, let’s understand the three phases of RCM.
Three Phases of RCM and How RPA Can Help Automate Each Phase?
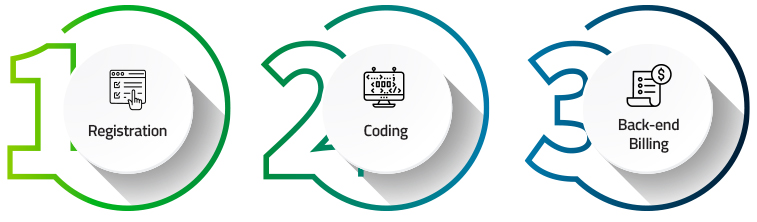
PHASE 1 - REGISTRATION
The RCM begins with pre-registration that is collecting information, such as insurance coverage before a patient arrives for inpatient or outpatient procedures. Next, comes the registration where the patient data is collected to establish a medical record number and meet various regulatory, financial and clinical requirements.
RPA can speed up phase 1 by eliminating the manual work required in gathering information, reviewing documents and managing files, and in creating a streamlined end-to-end process and subprocess applications for patient onboarding and registration. It can also automate the appointment schedules and can verify two to four days prior to an appointment.
PHASE 2 - CODING
Phase 2 is all about checking patient eligibility, benefits verification and claim submission. First comes the charge capture that is rendering medical services into billable charges. Then, comes the insurance utilization review where the necessity of medical services is examined. After that, comes the coding stage where the diagnosis and procedure services are coded for ease of understanding and making things less complicated. Lastly, a preauthorization is carried out which is confirming with the health insurer whether the prescription medication, procedure, service or equipment is medically necessary (except during medical emergencies), and finally, the claims of billable fees to insurance companies are submitted.
With RPA, every step of phase 2 that is extremely time-consuming can be automated. Humans can be freed for other vital tasks by automating checking, matching, reconciliation and calculations while coding including; the submission of claims into insurance portals by RPA.
PHASE 3 - BACK-END BILLING
The job does not end at claim submission. There are quite a few after procedures like remittance processing which requires extreme manual intervention in reviewing the amount approved, paid, disallowed, deductible, co-insurance, co-payments, etc., and performing data-entry of financial applications up to rejecting, ignoring or losing claims which is the hard part. Then, insurance follow-up and payment collections are carried out which again consumes a lot of time due to the repetitive accounting tasks, reconciliations, and payment updates within patient accounting systems. And the last step is reporting that involves generating a range of detailed reports including financial data, management information and key performance indicators to see if your team is meeting benchmarks.
A human error in claims submission processes, billing and coding systems can affect a patient's treatment as well as the revenue generation for the healthcare organization, therefore employing RPA into RCM is a must if you want to keep costs down and focus on improving patient outcomes. With RPA, care providers can achieve higher rates of clean (error-free) claims and fewer past-due patient payments, resulting in higher revenue and profits and lower expenses through automation of billing tasks.
Since 90% of claim denials are avoidable; effective prevention of claim denial can be obtained by uncovering patterns in denied claims, generating reports that provide detailed insight into an organization’s finances and performance indicators and thus helping recover lost revenue. RPA software bots can speed up the payment process by sending billing reminders via email and text messages with a direct link to payment portals.
Benefits of Employing RPA Process Robots in RCM
It may appear confusing how to get started with RPA or using it in which phase will be more beneficial? Questions like, should RPA be applied only in the pain points of RCM like denial management and pre-authorization where the fear of the claim getting rejected is the highest which happens a lot due to human errors? Or should it be used to automate entire Revenue Cycle Management?
Well, remember RPA is not a solution for automating every revenue cycle process, nor will it eliminate all manual jobs, RPA simply acts as a support for lessening the load on healthcare and in speeding up the processes without any errors. Therefore, RPA in RCM will give you the benefit of :
- Creating a 24/7 virtual workforce
- Eliminating human error and increasing standardization
- Expediting the retrieval process and cost estimate generation
- Speeding up pre-authorisation i.e. gathering claim information and feeding it directly into the HIS (Health Information System).
- Enhancing patient communication
- Reducing manual data entry
- Opportunities to review revenue shortfalls
- Providing insights on why a claim was denied including correcting and tracking unpaid claims
- Ensuring proper reimbursement for patients
- Defining a patient’s insurance status and copay requirements
- Increasing efficiency by integrating third-party tools
- Improving the consumer experience
What are the Challenges in Revenue Cycle Management?
It is important to maintain a strong revenue cycle for hospitals and healthcare to sustain performance but, there are quite a couple of challenges that can make it challenging to keep errors and delays out of the process. Let's peek into some of the top challenges in RCM.

How to Build Your RPA Center of Excellence?
Automating RCM using RPA software bots doesn’t mean eliminating humans and allowing robots to do the job, in fact, you will need an RPA CoE - which is a way to deeply embed RPA into organizations and redistribute accumulated knowledge and resources across future deployments.
So, to achieve an RPA CoE, you need to do the following:
Step 1: Set up a highly-skilled Robotic Operating Team consisting of RPA Sponsor, RPA Champions, RPA Change Manager, RPA Business Analyst, RPA Developer, RPA Solution Architect, RPA Infrastructure Engineer, RPA Supervisor, and RPA Service Support.
Step 2: Establish a scalable, functional and technical environment which involves defining resources and tools required for RPA implementation.
Step 3: Articulate an effective governance model. Certain guidelines must be established for the assessment, design, development and deployment of robots as well as in prioritizing automation activities and in assigning roles and responsibilities.
Step 4: Enable RPA CoE and measure results. After finishing your RPA setup, launch it and analyze if it is helping in achieving the desired results i.e. increased clean claims rates, decreased days in accounts receivable, decreased denials related to prior authorization or benefits and eligibility, operating cash flow etc. If it is, then have a growth plan ready to scale up further and thus sustain and develop your RPA expertise throughout the enterprise.
Wrapping up
Looking at the present scenario, the way our healthcare industry is loaded due to the deadly pandemic, RPA appears to be an excellent cure for the healthcare to sustain and survive and RPA in RCM; will make it further easier as the complexity of non-medical works gets eliminated after automation.
From all the analysis so far, it is clear that RPA in RCM can improve speed, performance and accuracy of the healthcare industry and we hope that the prediction of the global revenue cycle management (RCM) market of reaching USD 65.2 billion by 2025 definitely comes true.
Categories
Most popular
- Data Extraction challenges from Semi-Structured & Unstructured data source and how to overcome it
- The Scope of Healthcare Automation in Telehealth and Telemedicine
- Transforming Enterprise Business Management with Cognitive Robotics Process Automation
- How to Build an Intelligent Automation Strategy
- Automation Potential in Claims Processing
- Role of RPA in Revolutionizing Revenue Cycle Management of Healthcare
- The 7 major pitfalls to be avoided when implementing Robotic Process Automation
- Everything you need to know about Agile Process Management Solutions



